Airway management in patients with suspected or confirmed cervical spine injury
Recommendations
- Attempts should be made to minimise cervical spine movement during pre-oxygenation and facemask ventilation (Grade D; weak recommendation).
- When a simple manoeuvre is required to maintain an airway, jaw thrust should be used rather than head tilt plus chin lift (Grade D; weak recommendation).
- If tracheal intubation through a supraglottic airway device (SAD) is indicated, there is no specific device that is clearly superior in reducing cervical spine movement or successful tracheal intubation. Clinicians should use supraglottic airway devices that are familiar and available to them (Grade D; strong recommendation).
- Second-generation SADs should be considered in preference to first-generation SADs (Grade D; strong recommendation).
- Where possible, videolaryngoscopy should be used for tracheal intubation in patients with suspected or confirmed cervical spine injury (Grade A; moderate recommendation). We are unable to recommend a particular type of videolaryngoscope or a specific type of blade.
- Clinicians who perform tracheal intubation in patients with suspected or confirmed cervical spine injury should receive regular training in the use of videolaryngoscopy with cervical spine immobilisation (Grade D; weak recommendation).
- Clinicians should consider using an adjunct such as a stylet or bougie when performing tracheal intubation in a patient whose cervical spine is immobilised (Grade D; weak recommendation).
- During tracheal intubation attempts, a semi-rigid or rigid cervical collar should be removed, which can be done most easily by only removing the anterior part of the collar; this will also help minimise any movement to the cervical spine (Grade D, weak recommendation).
- Multidisciplinary planning, preparation and optimisation of human factors should be considered before airway management in patients with suspected or confirmed cervical spine injury (Grade D; weak recommendation).
Downloads and links
GUIDELINES
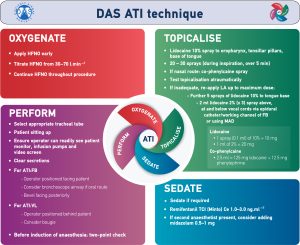
DAS guidelines for awake tracheal intubation (ATI) in adults
Difficult Airway Society guidelines (2019) for awake tracheal intubation (ATI) in adults.
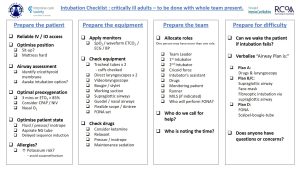
Guidelines for the management of tracheal intubation in critically ill adults
These guidelines (2017) describe a comprehensive strategy to optimize oxygenation, airway management, and tracheal intubation in critically ill patients, in all hospital locations.

Airway management in patients with suspected or confirmed cervical spine injury
Guidelines (2024) from the Difficult Airway Society (DAS), Association of Anaesthetists (AoA), British Society of Orthopaedic Anaesthetists (BSOA), Intensive Care Society (ICS), Neuro Anaesthesia and Critical Care Society (NACCS), Faculty of Prehospital Care and Royal College of Emergency Medicine (RCEM)
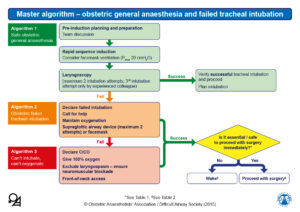
Management of difficult and failed intubation in obstetrics guidelines
This page hosts the Obstetric Anaesthetists’ Association and Difficult Airway Society’s 2015 guidelines for the management of difficult and failed tracheal intubation in obstetrics.
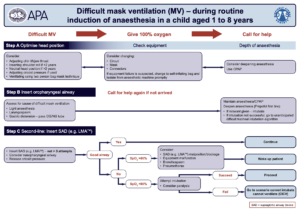
Paediatric difficult airway guidelines
The Paediatric Airway Guidelines Group, comprised of the Association of Paediatric Anaesthetists and the Difficult Airway Society, liaising with the RCoA, produced three algorithms relating to the management of the unanticipated difficult airway in children aged 1 to 8 years.
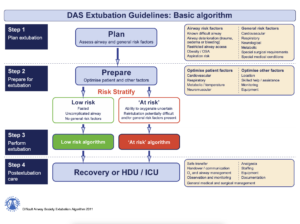
Management of tracheal extubation guidelines
The Difficult Airway Society has developed guidelines (2011) for the safe management of tracheal extubation in adult perioperative practice. The guidelines discuss the problems arising during extubation and recovery and promote a strategic, stepwise approach to extubation. They emphasise the importance of planning and preparation, and include practical techniques for use in clinical practice and recommendations for post-extubation care.
DAS guidelines for management of unanticipated difficult intubation in adults
The Difficult Airway Society 2025 guidelines for management of unanticipated difficult intubation in adults. This was the result of three years of diligent work by our guidelines development team.

Management of haematoma after thyroid surgery guidelines
DAS, BAETS & ENT UK consensus guidelines (2021) for management of haematoma after thyroid surgery. Written in collaboration with our surgical and nursing colleagues, we hope they will improve patient safety, whilst promoting teamwork and organisational preparedness.
Guidelines
The DAS difficult airway guidelines are the de facto standard in managing patients with difficult airway not only in UK but also in many other
